Drugs that relax smooth muscles. Antispasmodics
Yu. Belousov, Dr. honey. sciences, prof.
Spastic reactions accompany a significant number of diseases.b In this
Due to this, symptomatic antispasmodic therapy becomes very relevant.
Antispasmodics are widely used in diseases of the gastrointestinal tract, in
in particular with irritable bowel syndrome, with urological diseases,
spastic dyskinesias in gynecology.
Table. Classification of myotropic antispasmodics
To myotropic antispasmodics, or myolytics, which are widely used,
include: drotaverine (no-shpa), mebeverine, papaverine, otilonium bromide.
Myolytics lower smooth muscle tone by directly influencing biochemical
intracellular processes. They either lead to an increase in intracellular cAMP
or decrease in intracellular cGMP. cAMP activates the release of Ca++ from the cell and its
deposition, which leads to a decrease in the contractility of the cell. cGMP,
on the contrary, it increases contractility due to the stimulation of the release of Ca ++ from the depot.
Papaverine is an opium alkaloid that has myotropic antispasmodic action on the
smooth muscle intestines, bile ducts and urinary tract, especially
with spasms. Unlike other alkaloids, opium does not affect the central nervous system.
According to modern concepts, papaverine inhibits phosphodiesterase (PDE) in muscles,
which leads to an increase in the concentration of cAMP and associated with its accumulation
relaxation of smooth muscles. On the other hand, papaverine tends to
action similar to calcium antagonists.
Papaverine has a maximum antispasmodic effect on the colon, further
in descending order of effect: on the duodenum, antrum.
Papaverine is well absorbed from the gastrointestinal tract, may accumulate
in the liver and adipose tissue, extensively metabolized in the liver by microsomal
enzymes by conjugation with phenol, further excretion is carried out
by the kidneys by 60% in the form of metabolites, the rest is excreted unchanged.
Side effects: nausea, anorexia, diarrhea or constipation, malaise, headache
pain, dizziness, allergic skin reactions, rarely jaundice. At
parenteral administration, papaverine disrupts atrioventricular conduction and
can cause heart block.
Drotaverine (no-shpa) - antispasmodic myotropic action; on
activity is superior to papaverine.
The mechanism of action of drotaverine has been studied for many decades. He
associated with a change in the intracellular content of cyclic adenosine monophosphate
(cAMP) - a regulator of muscle tone. Drotaverine blocks a specific enzyme
phosphodiesterase, which degrades cAMP. Recent studies have shown that
PDE enzyme is represented by numerous isoenzymes (PDE I-VII), which
are located in different tissues and perform different functions. Drotaverine has
the highest selectivity of action against PDE IV (cAMP-sensitive), which
and is manifested by the accumulation of intracellular cAMP and a decrease in contractile
cell abilities. In addition, drotaverine has other mechanisms of action:
has the effects of calcium antagonists, blocks Na + channels (table). Together with
meanwhile, drotaverine is completely devoid of anticholinergic activity. Therefore, among
of all known groups of antispasmodics, no-shpa is one of the most
safe and well tolerated drugs.
After oral administration, drotaverine is well and rapidly absorbed, bioavailability
is 65%, and the maximum concentration in the blood is reached within 1 hour.
Drotaverine is highly associated with plasma proteins (95-98%); volume
distribution is large. Drotaverine penetrates well into various tissues: the central nervous system,
adipose tissue, myocardium, lungs, kidneys, liver, wall of the urinary and bile
bladder, intestines, vascular wall. Elimination is carried out slowly, per day
about 25% of the substance is eliminated, which is the result of the biliary pathway
excretion (up to 50%) and the presence of enterohepatic circulation. Drotaverine completely
metabolized in the liver with the formation of numerous metabolites. Period
half-life is 16 hours.
In order to improve the drug, a new dosage form -
no-shpa forte, with a high content of drotaverine hydrochloride (80 mg).
Side effects: with the introduction of a feeling of heat, sweating, dizziness,
tachycardia.
Antispasmodics of myotropic action also include calcium antagonists.
Calcium antagonists have an antispasmodic effect by blocking
slow voltage-gated calcium channels in smooth muscle
gastrointestinal tract.
Calcium antagonists also have little effect on receptor-dependent calcium channels,
therefore, they have a predominant effect in the duodenum 12. About 40%
tonic contractions of the colon are resistant to calcium antagonists, tk.
are carried out due to the mobilization of Ca ++ from intracellular depots. Antagonists
calcium cannot block the release of Ca++ from the depot.
Of the calcium antagonists, the antispasmodic effect of verapamil is 2-3 times stronger,
than nifedipine or diltiazem. Verapamil has an antispasmodic effect in
12 duodenal ulcer in concentrations much lower than required for
implementation of cardiovascular effects. Antispasmodic efficacy
calcium antagonists significantly decreases in the direction from upper to lower
sections of the gastrointestinal tract.
Currently, another myotropic antispasmodic with high
selectivity for the lower gastrointestinal tract - otilonium bromide.
Otilonium bromide (spasmomen) - myotropic antispasmodic, quaternary
ammonium compound, more active than papaverine. Mechanism of action of otilonium bromide
associated with the regulation of the level of intracellular Ca ++: it prevents both the entry of Ca ++
from the extracellular space, and blocks the mobilization of Ca ++ from the depot. This
the mechanism is of greatest importance in colonic contractions. Wherein
otilonium reduces both the amplitude and frequency of contractions, in contrast to
papaverine, which to a greater extent reduces the amplitude of contractions of the thick
intestines. Anticholinergic properties are weak and clinical significance not
have.
Otilonium bromide, unlike all other antispasmodics, is
highly selective agent due to the peculiarities of pharmacokinetics.
It is practically not absorbed after oral administration; is not subject to absorption.
more than 5% of the drug and 97% is excreted unchanged through the gastrointestinal tract.
Therefore, otilonium bromide acts exclusively locally (in the intestines) and has no
no systemic effects, incl. side effects.
Otilonium bromide due to the mechanism of action is the most effective in
increased motor activity of the colon, which is more often observed in the syndrome
irritable bowel with diarrhea.
Otilonium bromide is prescribed 40 mg 2-3 times a day before meals.
Otilonium bromide has excellent long-term tolerance in contrast to
from other antispasmodic drugs.
Thus, clinicians have several antispasmodic agents at their disposal.
drugs with sufficient efficacy and a wide profile
security.
Antispasmodics(antispasmodics), lek. in-va, causing a decrease in tone or elimination of spasm of smooth muscles and ext. organs (gastrointestinal tract, bronchi, uterus, biliary and urinary tracts, etc.). Spasmolytic. St. you have drugs that affect decomp. regulation of smooth muscle tone. There are neurotropic (act on the nervous system) and direct myotropic (act on muscles) antispasmodics, but some lek. in-va can be attributed simultaneously to both groups. Among neurotropic antispasmodics, central (, sedatives,) and peripheral (,) actions are distinguished.
Spasmolytic. effect of antispasmodics center. actions associated with limiting the flow of nerve impulses from the center. nervous system to the performer authorities. Peripheral neurotropic antispasmodics block or stimulate the corresponding ones in the execution. organs and. For example, anticholinergic drugs lower the tone or eliminate spasm of the gastrointestinal tract with peptic ulcer stomach and duodenum; stimulators of b 2 -adrenergic receptors reduce spasm of bronchial muscles in obstructive bronchopulmonary diseases.
The mechanisms of action of myotropic antispasmodics have not been fully elucidated. It is believed that these drugs affect the biochem. and biophys. p-tion, accompanying muscle contraction and regulating the content of cyclic. in smooth muscle, movement of Na +, K + and Ca 2+, formation or release from tissue depots of endogenous biologically active in-in(, etc.), changing the tone of smooth muscles and ext. organs.
Spasmolytic. St. you also have drugs from the group of so-called. Ca 2+ antagonists. The mechanism of their action is associated with the ability to inhibit the entry into the smooth muscle of Ca 2+ necessary for muscle contraction and, in connection with this, lower myofibrillar, which leads to a decrease in the utilization of energy-rich muscles and, consequently, to its relaxation. Ca 2+ antagonists include derivatives of phenylalkylamine (eg, verapamil), dihydropyridine (, or; f-la I), benzothiazepine (; II), (, or, III; lidoflazin, IV).
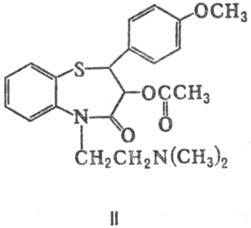
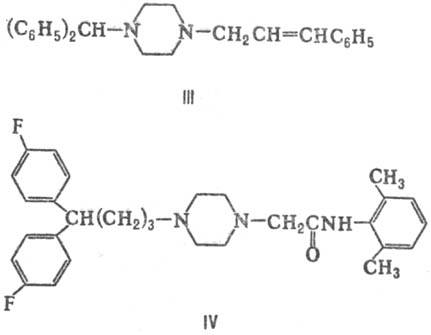
A number of myotropic antispasmodics has an elect. action on the tone of smooth muscles of certain organs or vascular areas. Among them, we distinguish w-va: coronary-expanding (antianginal w-va, coronary lytics), improving cerebral and peripheral. (peripheral vasodilators) blood circulation, bronchodilators (bronchodilators, bronchodilators), lowering the tone of the uterus (to-colytic agents), etc. Coronary dilating antispasmodics are org. and inorg. and -nitroglycerin, C 4 , (V), (CH 3) 2 CHCH 2 CH 2 ONO, NaNO 2, etc. Most of the drugs in this group are used in the form of the so-called. prolonged lek. forms, to-rye gradually isolated in the active in-in. Spasms of the brain reduce, in particular, derivatives of vincamine to-you - natural (devincan; VI) and synthetic (; VII). Peripheral vasodilators include the phthalazine derivative ( , or hydralazine; VIII) and Na 2 .
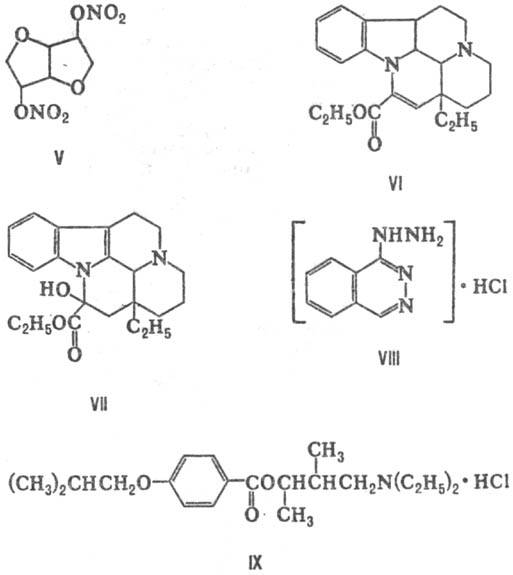
Non-selective myotropic antispasmodics include, for example, and carboxylic to-t [ (C 6 H 5) 2 CHC (O) S (CH 2) 2 N (C 2 H 5) 2, (C 6 H 5) 2 CHC (O)S(CH 2) 2 N(C 3 H 7) 2 , (IX)], derivatives ( , ; X), (
